Stem Cell Breakthrough To Transform Transplants: Melbourne researchers have made a world first breakthrough into creating blood stem cells that closely resemble those in the human body. And the discovery could soon lead to personalised treatments for children with leukaemia and bone marrow failure disorders.
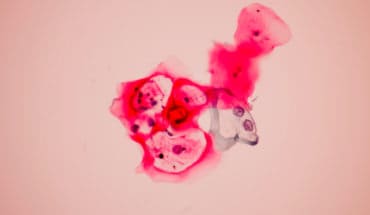
The research, led by Murdoch Children’s Research Institute (MCRI) and published in Nature Biotechnology, has overcome a major hurdle for producing human blood stem cells, which can create red cells, white blood cells and platelets, that closely match those in the human embryo.
MCRI Associate Professor Elizabeth Ng said the team had made a significant discovery in human blood stem cell development, paving the way for these lab grown cells to be used in blood stem cell and bone marrow transplants.
“The ability to take any cell from a patient, reprogram it into a stem cell and then turn these into specifically matched blood cells for transplantation will have a massive impact on these vulnerable patients’ lives,” she said.
“Prior to this study, developing human blood stem cells in the lab that were capable of being transplanted into an animal model of bone marrow failure to make healthy blood cells had not been achievable. We have developed a workflow that has created transplantable blood stem cells that closely mirror those in the human embryo.
“Importantly, these human cells can be created at the scale and purity required for clinical use.”
In the study, immune deficient mice were injected with the lab engineered human blood stem cells. It found the blood stem cells became functional bone marrow at similar levels to that seen in umbilical cord blood cell transplants, a proven benchmark of success.
The research also found the lab grown stem cells could be frozen prior to being successfully transplanted into the mice. This mimicked the preservation process of donor blood stem cells before being transplanted into patients.
MCRI Professor Ed Stanley said the findings could lead to new treatment options for a range of blood disorders.
“Red blood cells are vital for oxygen transport and white blood cells are our immune defence, while platelets cause clotting to stop us bleeding,” he said. Understanding how these cells develop and function is like decoding a complex puzzle.
“By perfecting stem cell methods that mimic the development of the normal blood stem cells found in our bodies we can understand and develop personalised treatments for a range of blood diseases, including leukaemias and bone marrow failure.”
MCRI Professor Andrew Elefanty said while a blood stem cell transplant was often a key part of lifesaving treatment for childhood blood disorders, not all children found an ideally matched donor.
“Mismatched donor immune cells from the transplant can attack the recipient’s own tissues, leading to severe illness or death,” he said.
“Developing personalised, patient-specific blood stem cells will prevent these complications, address donor shortages and, alongside genome editing, help correct underlying causes of blood diseases.”
Professor Elefanty said the next stage, likely in about five years with government funding, would be conducting a phase one clinical trial to test the safety of using these lab grown blood cells in humans.
Riya was diagnosed at the age of 11 with aplastic anaemia, a rare and serious blood disorder where the body stops producing enough new blood cells.
Due to the condition, Riya needed regular platelet and blood transfusions to get her blood cell count up.
A bone marrow transplant was recommended due to the amount of transfusions she was having and the concerns around possible long-term complications.
But they struggled to find a perfectly matched donor. Despite being a half match, Riya’s mother, following specialist advice, became her donor.
Read more about Riya’s recovery from a bone marrow transplant.
Prof Elefanty, Prof Stanley and Associate Professor Ng are also Principal Investigators at the Melbourne node of the Novo Nordisk Foundation Center for Stem Cell Medicine (reNEW), a global consortium, which aims to pave the way for future stem cell-based treatments.
Researchers from the University of Melbourne, Peter MacCallum Cancer Centre, University of California Los Angeles, University College London and the University of Birmingham also contributed to the findings.
Publication: Elizabeth S. Ng, Gulcan Sarila, Jacky Y. Li, Hasindu S. Edirisinghe, Ritika Saxena, Shicheng Sun, Freya F. Bruveris, Tanya Labonne, Nerida Sleebs, Alexander Maytum, Raymond Y. Yow, Chantelle Inguanti, Ali Motazedian, Vincenzo Calvanese, Sandra Capellera-Garcia, Feiyang Ma, Hieu T. Nim, Mirana Ramialison, Constanze Bonifer, Hanna K. A. Mikkola, Edouard G. Stanley and Andrew G. Elefanty. ‘Long-term engrafting multilineage hematopoietic cells differentiated from human induced pluripotent stem cells,’ Nature Biotechnology. DOI: 10.1038/s41587-024-02360-7
*The content of this communication is the sole responsibility of MCRI and does not reflect the views of the NHMRC.
- New lipid-based pathway discovered as key to memory formation - 25th June 2025
- Crucial link could explain how Alzheimer’s takes hold - 25th June 2025
- Understanding Your Mind Can Improve Daily Life - 25th June 2025