We would all like to see the end of terminal cancer. A non-survivable brain cancer killed my mother in a few short weeks. Last month, I said goodbye to a friend who died of a rare kind of blood cancer when she was just 55. Another friend has been diagnosed with stage 4 breast cancer, but we are all hopeful that ground-breaking treatment will give her plenty of time to watch her children grow up.
So, I was one of many people who reacted with joy and relief to news that scientists are developing immunotherapy drugs that seem to be having real impact on patients with terminal disease.
Headlines like ‘the living drug that could wipe out cancer’ and ‘miracle recovery’ suggested that breakthroughs announced at the recent American Association for the Advancement of Science conference in the US were ‘unprecedented in medicine’. In one study, more than half of the terminally ill blood cancer patients experienced complete remission in a clinical trial. In another study, 94 per cent of patients with acute lymphoblastic leukaemia saw symptoms disappear without trace.
But what is the truth behind the headlines? After careful looking at the facts and talking to leading cancer experts, I am now taking a more cautious view. Yes, immunological drugs, created by taking immune cells from patients and genetically reengineering them so that they target particular cells, will play an important role in future, but there is a long way to go before there are going to be any genuine miracles.
‘It’s not the death of terminal cancer yet but it is promising’ agrees Dr Alan Worsley, the senior science information officer at Cancer Research UK. ‘So far, the treatments have been used as a last resort when standard treatments have failed and it is for blood cancers only.’
Patients who have done well in trials may no longer have active cancer, but they also have severely compromised immune systems. The reengineered cells can’t be removed once they are in the body so they continue their campaign against cells that may now be healthy. ‘For a couple of hundred patients, this is a great plan C,’ says Dr Worsley.
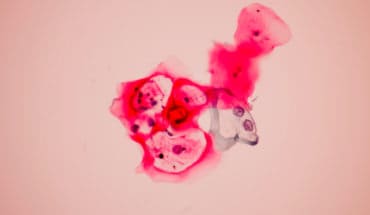
The real challenge is now to adapt the technology so that it can be used on more than ‘liquid’ cancers and work for solid tumours too. Modified T-cells, which were used in the trials, only patrol the blood and so far, there is no way to get them efficiently into other major organs and systems of the body where many cancers thrive.
The genetically modified immune cells also need to be much delicate operators. A kill switch must be developed to stop them in their tracks when they have done their job. Chemotherapy may be unpleasant but you can stop the drugs immediately by removing the catheter. Modified T cells march on, killing cells which have the marker whether they are cancerous or healthy.
And much more work needs to be done to identify the marker flags on cancer cells which the genetically altered immune cells can target. Many research teams around the world are working to establish what these tell-tale markers are.
‘It’s going to be a powerful weapon in the future but there is a lot more work that needs be done and we need to build in as many safeguards as possible,’ says Dr Worsley.
There is no doubt that we badly need to bolster our armoury against cancers of all types.
More people are being diagnosed with cancer than ever before – around 352,000 people were diagnosed with cancer in 2013 in the UK compared to 253,000 20 years ago, according to Cancer Research UK and that figure is expected to increase to more than 425,000 by 2030.[RM Strategic Plan 2014/2015.]
The good news is that survival rates are increasing dramatically. Over the last four decades, survival rates have doubled and today, half of the people diagnosed with cancer in the UK will survive for at least 10 years. [RM Strategic Plan 2014/2015]
But there is no room for complacency. Survival rates for some cancers, including pancreatic, lung and brain cancer remain low. And although many women with breast cancer can expect an excellent outcome, a proportion of women with breast cancer have poor life expectancy where treatments including surgery, chemotherapy and radiotherapy have failed.
It is these women who can look forward to a brighter future with the development of new drugs used in combination with existing treatments which improve the chances of halting the progression of their disease.
One exciting new drug treatment is the cyclin kinase inhibitors. Growth of hormone receptor positive breast cancer can be dependent on cyclin-dependent kinases 4 and 6, which promote a key step pathway in the phase of a cell cycle. Together with traditional hormone therapy drugs such as the aromatase inhibitors, the combined effect can be a powerful anticancer agent without the need for chemotherapy.
There are women diagnosed with Stage 4 breast cancer 10 years ago whose disease has not progressed thanks to these drugs which target cyclin-dependent kinases in cancer cells which are critical to cell division and thus tumour growth.
Palbociclib, developed by Pfizer for ER-positive and HER2 negative breast cancer, is a cyclin-dependent kinase therapy which has just been approved by the FDA in the USA. Trials have shown that, when used in combination with other drugs, Palbociclib offers women longer progression-free survival.
The issue is about balancing expense with effectiveness. Palbociclib costs in the region of £10,000 per month per patient and can only be accessed in the UK if you are on a clinical trial, on a Compassionate Use programme, or willing to pay privately from overseas. It is yet to be licensed in Europe. There is evidence that it may be useful at early stages of relapsed disease, avoiding more aggressive treatment, but many of these early stage patients will be fine without Palbociclib, which offers reassurance but is not necessarily a lifesaver.
- Biden Declines Second Term: Health Concerns - 23rd July 2024
- New catheter coating stops bacteria cells from swarming - 10th June 2024
- AI-designed catheters could dramatically reduce urinary tract infections - 10th June 2024