When it comes to treating pancreatic cancer, speed is of the essence. Pancreatic cancer is one of the deadliest forms of the disease and less that seven per cent of patients will survive longer than five years past their diagnosis. The reason for this is that diagnosis is often made when the disease is advanced and surgery is not an option.
But for those who could benefit from surgical removal of the tumour, swift intervention can make all the difference. A team at University Hospitals Birmingham NHS Foundation Trust has just successfully trialled a new ‘fast track’ system which reduces the average waiting time to surgery from two months to just over two weeks.
A team at University Hospitals Birmingham NHS Foundation Trust has just successfully trialled a new ‘fast track’ system which reduces the average waiting time to surgery from two months to just over two weeks.
Not only has this system, reported on in the HPB journal this week, increased the number of patients whose surgery was successful by 22 per cent, but it has also saved the NHS around £3200 per patient – a win/win in anyone’s book.
Pancreatic Cancer UK, which funded the pilot, says these results are incredibly exciting because if the pathway was rolled out UK-wide, each year it could see hundreds more patients having surgery which successfully removes their tumour. This is the one treatment for pancreatic cancer which can save lives. The charity says this would be a significant breakthrough for a cancer which has seen very little progress in treatments since the early 1970s.
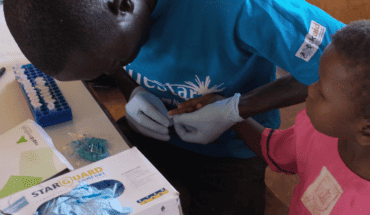
Consultant Hepatobiliary and Pancreatic Surgeon Keith Roberts and his team focused on ways of reducing the time it takes for eligible patients to have surgery, to see if this meant that more of those patients had their tumour successfully removed.
The team worked with hospitals to speed up referrals for patients and reorganised the way surgery was carried out. They also cut out a treatment generally given to patients before surgery for the symptom of jaundice (yellow skin or eyes or itchy skin). They reduced the time to surgery from an average of 65 days to 16 days. This meant that 97 per cent of patients who were eligible for surgery went on to have the treatment successfully, compared to a current average of 75 per cent of eligible patients.
The savings to the NHS were made by cutting out the treatment for jaundice before surgery, as well as reducing complications and hospital readmissions after surgery.
Keith Roberts, who is also a member of Pancreatic Cancer UK’s Medical Advisory Board, said: “We have shown that it is possible to create a much faster path to surgery for pancreatic cancer patients within the NHS, which could have a significant impact on survival. We carried out surgery earlier and on more patients, avoided unpleasant and costly pre-surgery treatment, and yet there was no significant increase in complications post-surgery. At University Hospitals Birmingham NHS Foundation Trust we hope to permanently fund the pathway, and I am sharing the results of our pilot far and wide, in the hope that more trusts will roll it out.”
Alex Ford, Chief Executive of Pancreatic Cancer UK, said: “These results are incredibly exciting. Surgery is the only treatment for pancreatic cancer that can save lives. If we can ensure that hundreds more patients have their tumour successfully removed each year, it could be a huge breakthrough in treatment.
“The exceptional element of this pilot is that it saved the NHS £3,200 per patient. If we could see this pathway rolled out across the board, those savings could be reinvested into specialist nurses who could make the journey to surgery even quicker. Those nurses would in turn be a game-changer for pancreatic cancer care, and create more savings for the NHS too. We urge NHS England and specialist health commissioners across the UK to take heed of these results and allow hundreds more patients each year to have potentially life-saving surgery far more quickly.”
Pancreatic Cancer UK gave the team at University Hospitals Birmingham NHS Foundation Trust a grant of £50,000 through its Clinical Pioneers Awards. The scheme funds innovative research in a clinical or community setting which can benefit current patients and their families, as well as bring about the breakthroughs in diagnosis, treatment and care which must be delivered
for the future.
- New lipid-based pathway discovered as key to memory formation - 25th June 2025
- Crucial link could explain how Alzheimer’s takes hold - 25th June 2025
- Understanding Your Mind Can Improve Daily Life - 25th June 2025