Can we eliminate the need for bone marrow donors? There is a chance that we can. At the moment, people who develop leukaemia, lymphoma and other blood diseases often need to undergo a hematopoietic stem cell transplantation (“HSCT”). This is because initial treatment of the disease (front-line therapy) often fails and the disease comes back.
Hematopoietic stem cells (HSC) are vital because they constantly regenerate the blood system giving rise (differentiating) into all types of blood cells such as red blood cells, white blood cells and platelets. Sometimes, patients get cells for the HSCT from close relatives (“related allogeneic transplantation”), who happen to be a match or by using donor data bases that can match them with strangers (“unrelated allogeneic transplantation”). The patient’s own HSC are wiped out with chemotherapy and replaced with the donated blood-forming stem cells which create healthy new blood cells free from disease.
Often, there is not a perfect match between a donor and a patient but physicians try and find the closest one possible. When a match is not perfect, a risk of rejection of the newly transplanted cells significantly grows.
Often, there is not a perfect match between a donor and a patient but physicians try and find the closest one possible. When a match is not perfect, a risk of rejection of the newly transplanted cells significantly grows.
There are several teams of researchers trying to find a way to eliminate the need for bone marrow donors altogether and instead use different types of cells derived from the patient in need of a transplant.
This work, to directly reprogram the patient’s own cells to create hematopoietic stem cells, (from which all cellular blood components are derived) has been going on for some time and has had some success. However, it is a very long and cumbersome process to produce HSC cells from a patient’s own cells and it looks like this may never be a practicable solution to the problem. We simply can’t seem to be able to get the newly formed HSC cells to replicate into the sufficient number of cells needed to form a viable HSCT.
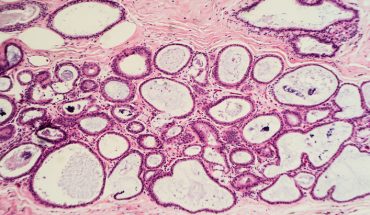
What I discovered when I was at Cornell University was that there is a small subset of postnatal hemogenic endothelial cells (“Hu-PHEC”) which survive in the liver and blood vessels of the umbilical cord and placenta into adulthood. It has been known for quite a while that in the fetus, similar cells produce first definitive HSC. It was accepted as a dogma that they either lose their ability to do this after birth or simply disappear. However, as it often happens in science, this was not entirely correct. Hu-PHEC can be isolated from postnatal tissues and made to generate HSC de-novo.
In animal experiments, we took purified and stimulated Hu-PHEC and transplanted them into immunocompromised mice. What we found was that the transplanted cells did engraft and created a healthy new human blood system in the recipient mice. What seemed to happen was that by putting them back into circulation within the body reactivated their ability to produce HSC cells as they do in utero. We don’t yet understand the mechanism but we are working on this and we need to work out a way to get enough cells for human transplantation.
Development of Hu-PHEC technology would create an opportunity to get rid of bone marrow/HSC donations. We would no longer have to go to a donor or a family member, but simply harvest some of these special post-natal hemogenic endothelial cells from the patient’s own body.
Another area of our research has been to develop a conditioning product which helps eliminate the patient’s diseased HSC with minimal collateral damage to the rest of the body. At the moment, patients undergo a rather terrible process of preparation for a HSCT. It involves chemotherapy and radiation and can seriously harm various unrelated healthy cells. In some cases, patients do not survive the conditioning process. We have developed a type of immune therapy which is a bi-specific antibody that redirects patient’s own immune cells to only attack and kill HSC. It leaves other cells alone, so does not damage reproductive system. This should mean that men and women undergoing conditioning in advance of a bone marrow transplantion would not need to undergo fertility saving treatment (no need to freeze sperm or eggs). This bi-specific antibody, which is filed for a world-wide patent, is much less dangerous and detrimental to health than current treatment options. We have proved its effectiveness in animal trials, but we are now hoping to move on to Phase 1 clinical trials
- Eliminating the need for bone marrow donors - 18th July 2017